Interprofessional Education - IPE
The team at Clinical Pattern has created the first Online Interactive Inter-Professional Simulation based on the assessment and management of a real client with traumatic brain injury. This interprofessional simulation combined with a 1 hour self-guided synchronous session for students from various professions allows for a cost and time efficient approach for programs and universities all over the world.
This simulation includes:
-
A client in the neurologic rehabilitation setting with traumatic brain injury
-
Introduction to each member of the rehabilitation team
-
Brief evaluation and treatment by members of the rehabilitation team including:
-
Physician
-
Nurse
-
Occupational Therapist
-
Physical Therapist
-
Speech language pathologist
-
Case manager
-
-
Team discussion to optimize patient care
Evidence suggests that Inter-Professional Care is a means to better health, better care and lower costs. Homeyer et al, discussed four primary arguments for IPE (Inter-Professional Education):
- Development and promotion of inter-professional thinking and acting
- Acquirement of shared knowledge
- Promotion of beneficial information and knowledge exchange
- Promotion of mutual understanding
Why is it so hard to implement?
Major barriers of IPE are:
- Difficulty with coordination and harmonization of the curricula between professions
- Time intensive
- Space intensive
- High cost to develop simulations
- Limitations of paper cases to create a realistic and engaging experience for learners
With the continued challenge of the COVID-19 pandemic and the emerging value of online simulations (Pritchard et al, Carla et al, Bethea et al.), A team of clinicians and academic instructors were determined to plan, film and program a fully interactive, asynchronous inter-professional simulation. This online, interactive, asynchronous inter-professional learning experience has been tested in inter-university settings over the 2021 and 2022 academic years. Data from these experiences will be presented at the Association of Allied Health Professionals Annual Conference 2022 in Long Beach, California.
This resource has been made available to all allied health programs in the world to support Interprofessional Education academic efforts in this challenging time of professional higher education.
How do student participants rate this experience?
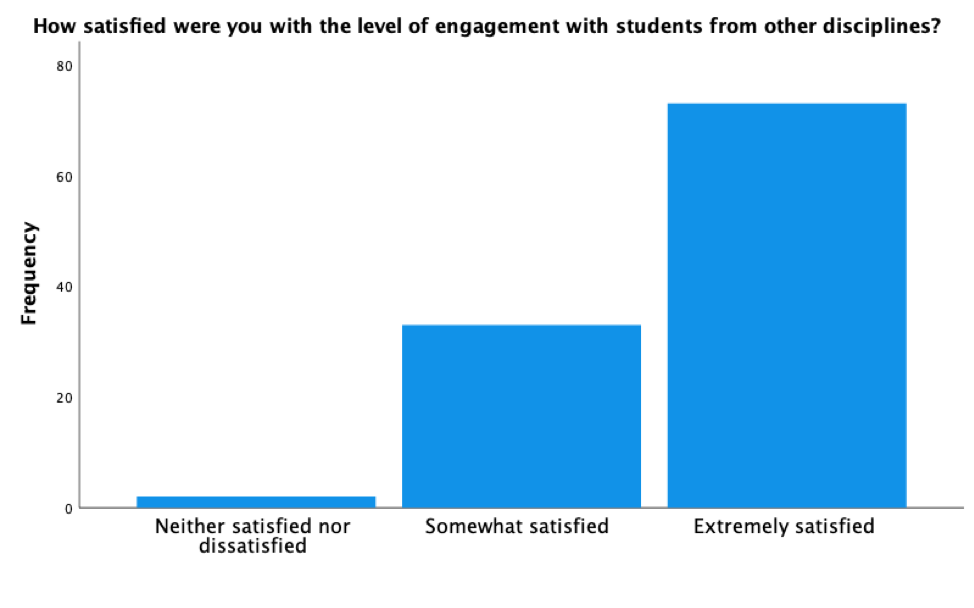
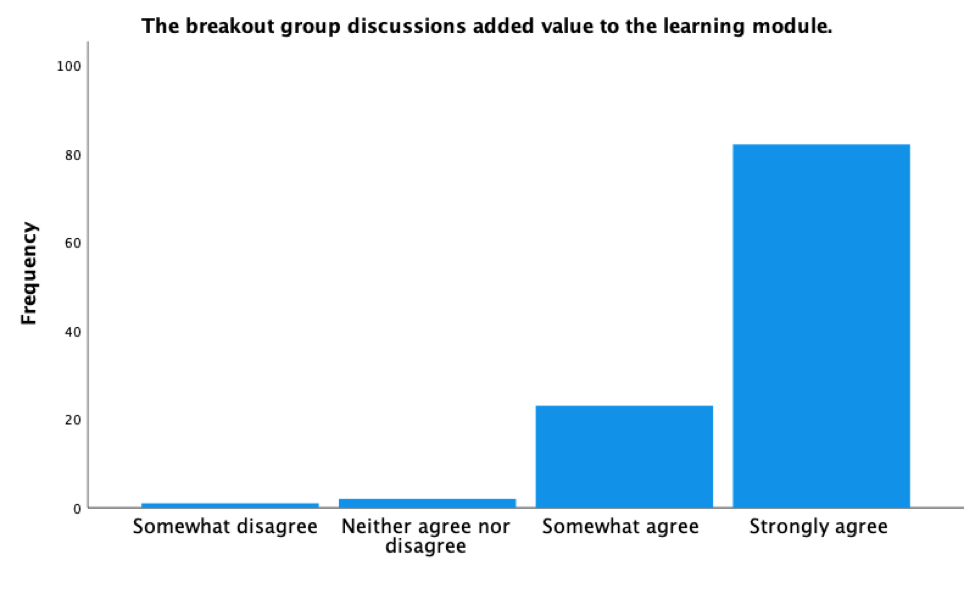
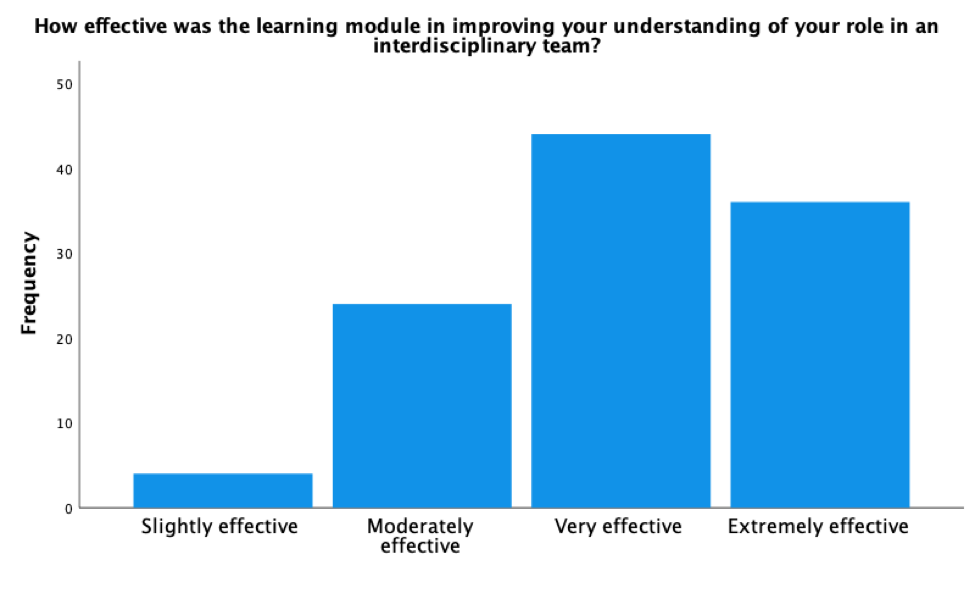
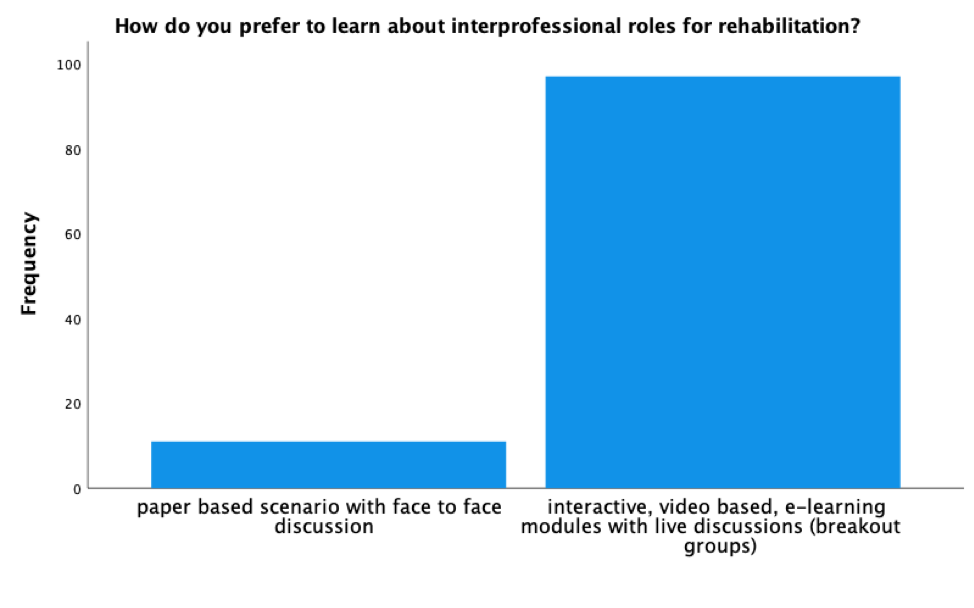
Results of our study demonstrate high levels of satisfaction from students using this modality to explore inter-professional practice in both the asynchronous use of the simulation and the1 hour face-to-face synchronous session between the OT/SLP programs at Indiana State University and the PT program at Azusa Pacific University:
- A total of 108 students from 3 professional programs (PT,OT, SLP) participated in the survey and the interactive IPE experience.
- 97.3% indicated they were either extremely satisfied (n = 73) or somewhat satisfied (n= 33) with the level of engagement with students from other professions.
- 89% of respondents indicated they preferred the e-learning modules with live breakout room discussions over paper-based, face-to-face scenarios.
All respondents reported the e-learning module was effective in improving their understanding of their role in an interdisciplinary team (Extremely effective 33%, Very effective 40.4% Moderately effective 22%, and slightly effective 3.7%)
How do I implement this between multiple programs and universities?
- Invite students from multiple programs to complete the simulation the week before the pre-scheduled online meeting (Asynchronous IPE)
- Invite students and faculty to syncronous discussion session on virtual meeting platform
- Prior to meeting day, pre-assign students from different professions to break out rooms to ensure that each room has an even spread of students from various disciplines
- On day of discussion, follow script in attached document to welcome everyone and set the agenda for the synchronous discussion session
- Break students into breakout room where they will use the discussion guide to self-lead the discussion
- After 30 minutes, reconvene the group for closing statements and faculty sharing experiences related to interprofessional collaboration
How much does this resource cost?
It is a free resource created to enhance interprofessional collaboration and to reduce faculty burden
References
- Bethea, D. P., Castillo, D. C., & Harvison, N. (2014). Use of Simulation in Occupational Therapy Education: Way of the Future? The American Journal of Occupational Therapy, 68(Supplement_2), S32-S39. doi:10.5014/ajot.2014.012716
- Carter, M. D. (2019). The effects of computer-based simulations on speech-language pathology student performance. Journal of Communication Disorders, 77, 44-55. doi:https://doi.org/10.1016/j.jcomdis.2018.12.006
- Dudding, C. C., & Nottingham, E. E. (2018). A National Survey of Simulation Use in University Programs in Communication Sciences and Disorders. Am J Speech Lang Pathol, 27(1), 71-81. doi:10.1044/2017_ajslp-17-0015
- Gaba, D. M. (2004). The future vision of simulation in health care. Qual Saf Health Care, 13 Suppl 1(Suppl 1), i2-10. doi:10.1136/qhc.13.suppl_1.i2
- Galloway, S. J., (2009) "Simulation Techniques to Bridge the Gap Between Novice and Competent Healthcare Professionals" OJIN: The Online Journal of Issues in Nursing,Vol. 14, No. 2, Manuscript 3. DOI: 10.3912/OJIN.Vol14No02Man03
- Gibbs, D. M., Dietrich, M., & Dagnan, E. (2017). Using high fidelity simulation to impact occupational therapy student knowledge, comfort, and confidence in acute care. The Open Journal of Occupational Therapy, 5(1). https://doi.org/10.15453/2168-6408.1225
- Henneman, E. A., Cunningham, H., Roche, J. P., & Curnin, M. E. (2007). Human patient simulation: teaching students to provide safe care. Nurse Educ, 32(5), 212-217. doi:10.1097/01.NNE.0000289379.83512.fc
- Herrera-Aliaga, E., & Estrada, L. D. (2022). Trends and Innovations of Simulation for Twenty First Century Medical Education. Front Public Health, 10, 619769. doi:10.3389/fpubh.2022.619769
- Lateef, F. (2010). Simulation-based learning: Just like the real thing. Journal of Emergencies, Trauma, and Shock, 3(4), 348-352. doi:10.4103/0974-2700.70743
- Sabus, C., & Macauley, K. (2016). Simulation in Physical Therapy Education and Practice: Opportunities and Evidence-Based Instruction to Achieve Meaningful Learning Outcomes. Journal of Physical Therapy Education, 30(1). Retrieved from https://journals.lww.com/jopte/Fulltext/2016/30010/Simulation_in_Physical_Therapy_Education_and.2.aspx
- Steadman, R. H., Coates, W. C., Huang, Y. M., Matevosian, R., Larmon, B. R., McCullough, L., & Ariel, D. (2006). Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med, 34(1), 151-157. doi:10.1097/01.ccm.0000190619.42013.94
- Singh, J.& Matthees, B. (2021) Facilitating interprofessional education in an online environment during the COVID-19 pandemic: A mixed method study. Healthcare, 9, 567. https://doi.org/10.3390/healthcare9050567
- Spaulding, E.M., Marvel, F.A., Jacob, E., Rahman, A. Hansen, B.R., Hanyok, L.A., Martin, S.S., & Han, H. (2021) Interprofessional education and collaboration among healthcare students and professionals: A systematic review and call for action. Journal of Interprofessional Care, 35(4), 612-621. https://doi: 10.1080/13561820.2019.1697214
- Bianchi, M., Bagnasco,A., Aleoa,G., Catania, G., Zaninia, M.P., Timmins, F., Carnevale,F., & Sasso, L. (2018) Preparing healthcare students who participate in interprofessional education for interprofessional collaboration: A constructivist grounded theory study protocol. Journal of Interprofessional Care, 32(2), 367-369. https://doi.org/10.1080/13561820.2017.1340877
- Council on Academic Accreditation in Audiology and Speech-Language Pathology. (2020). Standards for accreditation of graduate education programs in audiology and speech-language pathology (2017). Retrieved 9/7/2022 from https://caa.asha.org/siteassets/files/accreditation-standards-for-graduate-programs.pdf



